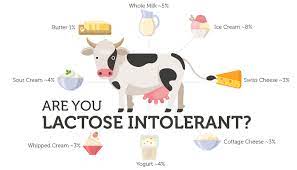
 Are you Lactose intolerant?
Are you Lactose intolerant?
Food intolerances causes a range of gut and systemic symptoms. The possibility that these conditions might be caused by lactose intolerance is often missed because it is not generally known how widely lactose is used as a food additive. For example in most tablets and medication lactose is often one of the ingredients. Also lactose is added to manufactured food and drinks and is often not mentioned on the package label. Lactose has about 1/6 of the sweetness of sucrose, unlike sucrose or glucose it is not metabolised effectively by yeast. Therefore lactose can be added to foods and drinks without causing a sickly sweet taste and without generating carbon dioxide or ethanol as a result of yeast metabolism.
Lactose is used as a Browning agent in bread and cakes, it is added to processed pork meats such as sausages on burgers and sometimes chicken meat. It is also added to soft drinks beers, lagers, breakfast drinks, dieting slimming products. As a result there is often confusion with regard to dietary advice because many people think that avoiding dairy products simply means avoiding milk and yogurt and cheese but don’t forget that if you have lactose intolerance you also probably should avoid chocolate ice cream and many sweet things as they often contain cream or milk!
Lactose, a disaccharide, is not normally absorbed directly from the gut, but is hydrolysed by the action of the brush border lactase into glucose and galactose, which are then absorbed by the enterocytes and passed into the hepatic portal blood supply. Interestingly since starting to look into the microbiomes of patients with the Flore test we have noticed that the majority of UK and Irish people dont have the microbe Streptococcus Thermophilus. This is the microbe that produces lactase the enzyme that breaks down lactose. Is it any wonder so that we have intolerances to dairy?
If the lactase is absent or insufficient for the dietary load of lactose then the non absorbed lactose will be passed through the lower small instestine and colon. This may result in an osmotic diarrhea all varying severity, along with cramps and flatulence, which are the symptoms of the condition known as lactose intolerance. Lactose intolerance is not an allergic condition but a digestive condition. All adult mammals, except for northern Europeans and certain other ethnic groups for example African Masai tribes even among these groups much of the activity is normally lost after weaning. Lactase malabsorption refers to the physiological consequences of lactase deficiency, which can for example be genetic or (secondary acquired, from intestinal damage caused by the microorganism Giardia Lambia or Rotavirus A infections where the integrity of the intestinal mucosa is compromised. Primary lactase deficiency is a rare and serious condition, resulting results in the inability to consume maternal milk or feed containing lactose.
Without adequate intestinal lactase activity, consumption of lactose results in its passage into the large intestine, which hydrogen, methane and other metabolites being generated by colonic bacteria. These metabolites include toxins, acetylaldehyde, dimethylglyoxal, formic acid, propane – 1,3- diol, indoles and skatoles. Lactose itself can also have toxic effects if absorbed directly into the bloodstream without hydrolysis in the intestine. These toxins act on ionic signaling pathways in the nervous, cardiovascular, skeletal, muscle and immune systems and it is now clear that their effects can cause a range of debilitating systemic symptoms, in addition to the well known gut symptoms, such as those associated with irritable bowel syndrome, eczema, asthma and osteoarthritis.
Lactose intolerance was formerly assessed by giving an oral dose of 50 grams of lactose equivalent to the lactose load in one liter of cows milk and then monitoring the plasma glucose for three hours. A normal response in this test is a rather modest rise in the plasma glucose, of greater than 1.2 MMOL, liter. The lactose tolerance test is now rarely carried out. Even in some control subjects with no known relevant history may exhibit some symptoms and fail to produce a significant rise in the plasma glucose showing the high prevalence of the condition.
A trial lactose free elimination diet may also provide useful for initial assessment of lactose intolerance but small bowel biopsy with the assay of brush border disaccharidase activities formerly provided the definitive diagnosis. Genetic testing based on an EDTA blood sample is now possible it gives information as to susceptability rather than the presence of the condition which being polymorphic in its genetics required investigation number of loci.
Our experience is that the comparison of breath levels of hydrogen and maintain before and after the consumption of lactose provides a convenient and practical way of detecting the condition called lactose intolerance. This is of considerable importance in the investigation of a number of chronic conditions and its increasing prevalence reflects the dietary load of lactose from manufactured foods as well as the extent of loss of brush border lactase in the human body.
Contact me to order this test for you 0868439979 or ei.tugruoyhtiwog@ofni



